A New Approach to Treating Non-Small Cell Lung Cancer: Direct Thrombin Inhibitors Block the Disease's Spread and Spontaneous Metastasis
*Corresponding Author:Received Date: Nov 09, 2023 / Published Date: May 12, 2025
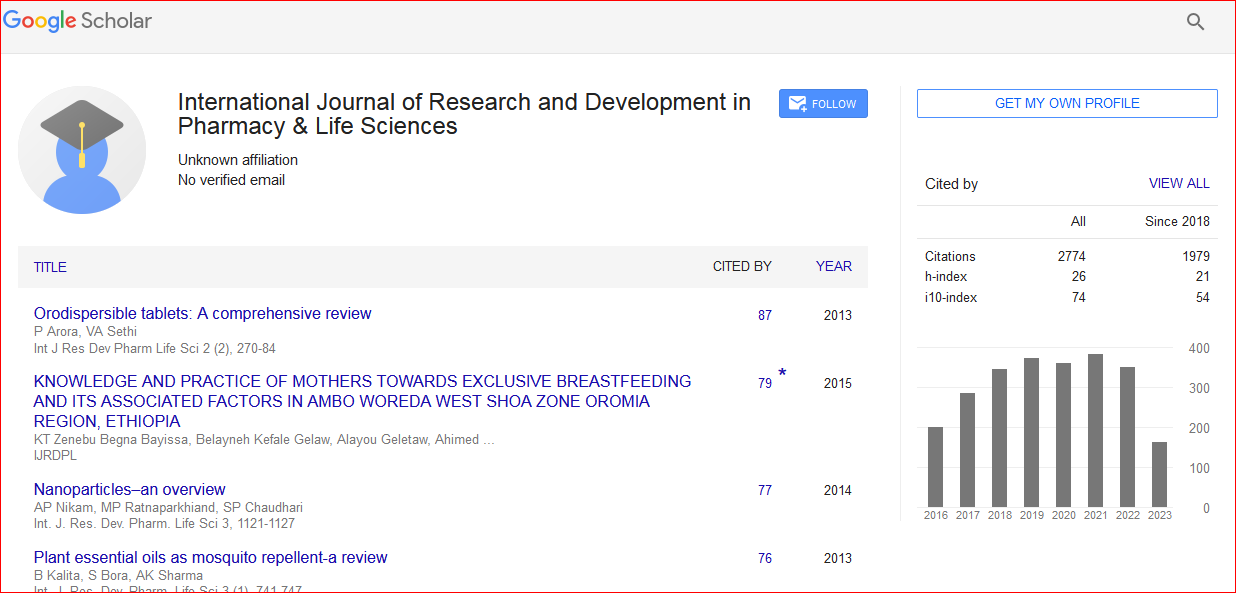
Citation: Sonwani HP, Sinha A (2025) A New Approach to Treating Non-small Cell Lung Cancer: Direct Thrombin Inhibitors Block the disease's Spread and Spontaneous Metastasis. Int J Res Dev Pharm L Sci 11: 273
Copyright: © 2025 Sonwani HP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Two potentially lethal effects of advanced cancer are cancer cachexia and cancer-associated thrombosis. However, there is still much to learn about the expression of thrombin in primary tumor tissues of Non-Small Cell Lung Cancer (NSCLC) and how this may relate to the prognosis of NSCLC patients. A clinical pathological examination was conducted to ascertain the correlation between the advancement of the cancer and thrombin. We assessed the impact of r-hirudin and Direct Thrombin Inhibitor Peptide (DTIP) on the advancement of cancer. Immunohistochemistry, immunofluorescence, and Western blotting were employed to investigate the mechanism of r-hirudin and DTIP inhibition. It was established how well DTIP and chemotherapy worked together therapeutically. The presence of thrombin in NSCLC tissues was strongly associated with clinicopathogenic characteristics and the patients' prognosis. Tumor growth was reduced by thrombin insufficiency. R-Hardin, one of the new thrombin inhibitors and DTIP, respectively, prevented in vitro cell invasion and metastasis. In an orthotropic lung cancer model, they prevented tumour development and metastasis, impeded cell penetration, and extended survival following tumour cell injection through the tail vein. Additionally, they prevented spontaneous metastases and angiogenesis from tumours that were subcutaneously injected. In PAR-1-deficient NSCLC cells, thrombin's stimulation of invasion and metastasis was eliminated. Tissue growth was suppressed by r-hirudin and DTIP via the thrombin-PAR mediated NF-κB and RhoA signalling cascades by suppressing the expression of MMP9 and DTIP prevented chemotherapy-induced resistance in mice and enhanced chemotherapy-induced growth and inhibition of metastasis. Thrombin contributes significantly when combined with PAR-1, to cancerous NSCLC. Anti-tumor therapy may make use of the anticoagulants r-hirudin and DTIP, or a combination of and DTIP prevented cell invasion and in vitro metastasis. In an orthotopic lung cancer model, they slowed the growth and spread of the tumours, prevented cell invasion, and increased the length of survival following tumour cell injection via the tail vein. They also prevented spontaneous metastases from tumours that were subcutaneously injected and angiogenesis. In NSCLC cells lacking PAR-1, thrombin's stimulation of invasion and metastasis was eliminated. Through the thrombin-PAR-pathway, rhirudin and DTIP prevented the growth of tumours. DTIP, two anticoagulants, in conjunction.